The changing role of the GP Receptionist

We all know that demand on GP surgeries has increased hugely in recent years. This is due to many factors, which include more work being done in the community rather than the hospital. Also, the backlog in hospital care means that patients need more ongoing support from their GP.
But what do these changes mean to those on the front line of our surgeries? In particular, how does it affect the receptionists who deal with patients’ calls and visits to surgeries on a daily basis.
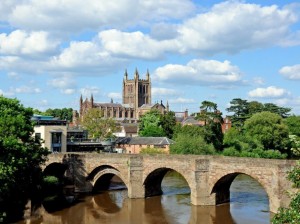
We caught up with Lucy Ridgway, Reception Manager at Nunwell Surgery in Bromyard to find out.
Lucy has been working for nine years in a reception role, the last six to nine months in the management role. Here's what she said:
How has the role of the Practice Receptionist changed over the years?
Covid changed things massively. Overnight we had to change completely and it was unsafe to allow patients in the surgery - we had to close the door and use an intercom system for people turning up at the surgery and we set up a portacabin so we could see anyone absolutely necessary after they were triaged by our Doctors.
On top of that, we have had to deal with the huge stress under which the NHS continues to operate. This has affected how we deal with patients. Nowadays, we are Care Navigators, trained to help patients to help themselves and to get them to the right place for their care more quickly. This is very different to the past when we just booked patients in to see their GP.
How can patients be reassured about the competency of receptionists to do this care navigating?
I have been in post for nine years and I’m still learning! Life changes constantly, both in terms of the NHS and outside. For a new receptionist there’s a lot to take on board, and they receive training in many different aspects. For example, how can pharmacists help, what is social prescribing, how patients can access help via NHS online and our own online consultancy service. This equips them effectively to signpost patients to the right professional for their needs.
Some patients can be reluctant to discuss personal issues with us. But we try to advise them that we’re not being nosey and that we’re only asking about the reason for their call so we can help them to get the most appropriate care.
What’s the most challenging part of your job?
Aggressive patients. We do try our best with all patients and it is difficult and upsetting when they become aggressive. Thankfully, we don’t have many and the surgery has a zero tolerance policy. Our management team is very supportive.
At the end of the day we’re people too, so there are also patient situations which are incredibly moving and can affect us.
And the best part of your job?
I know it sounds cheesy, but it’s helping people. Sometimes we can be the only ones who patients talk to in the day. There’s also the camaraderie and team working – everyone here is very suportive and will make you a nice cup of tea if you need it!
What one message would you most like to get across to patients?
That they don’t always need to see a GP and that other professionals may be more suitable to help them with their particular issue. Also, that we’re not just receptionists – there’s much more to our role than passing on calls/making appointments.
More Articles
For further information about any of these news stories, please email the Communications Team

Taurus Annual Report 2024/25
Taurus Healthcare has published its Annual Report for 2024/25. The report reflects a year of transformation…
Herefordshire chosen to help shape the future of local health and care
We’re excited to share that Herefordshire has been selected as one of just 43 areas in England…

Herefordshire GP Leaders Spotlighted in National NHS Confederation Webinar
Dr Lauren Parry, Medical Director, and Dr Nigel Fraser, Chairman of Herefordshire General Practice…
